BOISE, Idaho — As new COVID-19 cases continue to add up by the hundreds each day in Idaho, hospitals report that people infected with the coronavirus are filling inpatient beds in numbers not previously seen during the pandemic.
For some hospitals and clinics, the number of people needing care exceeds capacity in terms of available beds and available doctors and nurses.
Idaho's two northernmost health districts requested the activation of crisis standards of care, and the Idaho Department of Health and Welfare on Tuesday activated crisis standards for the Panhandle and North-Central districts.
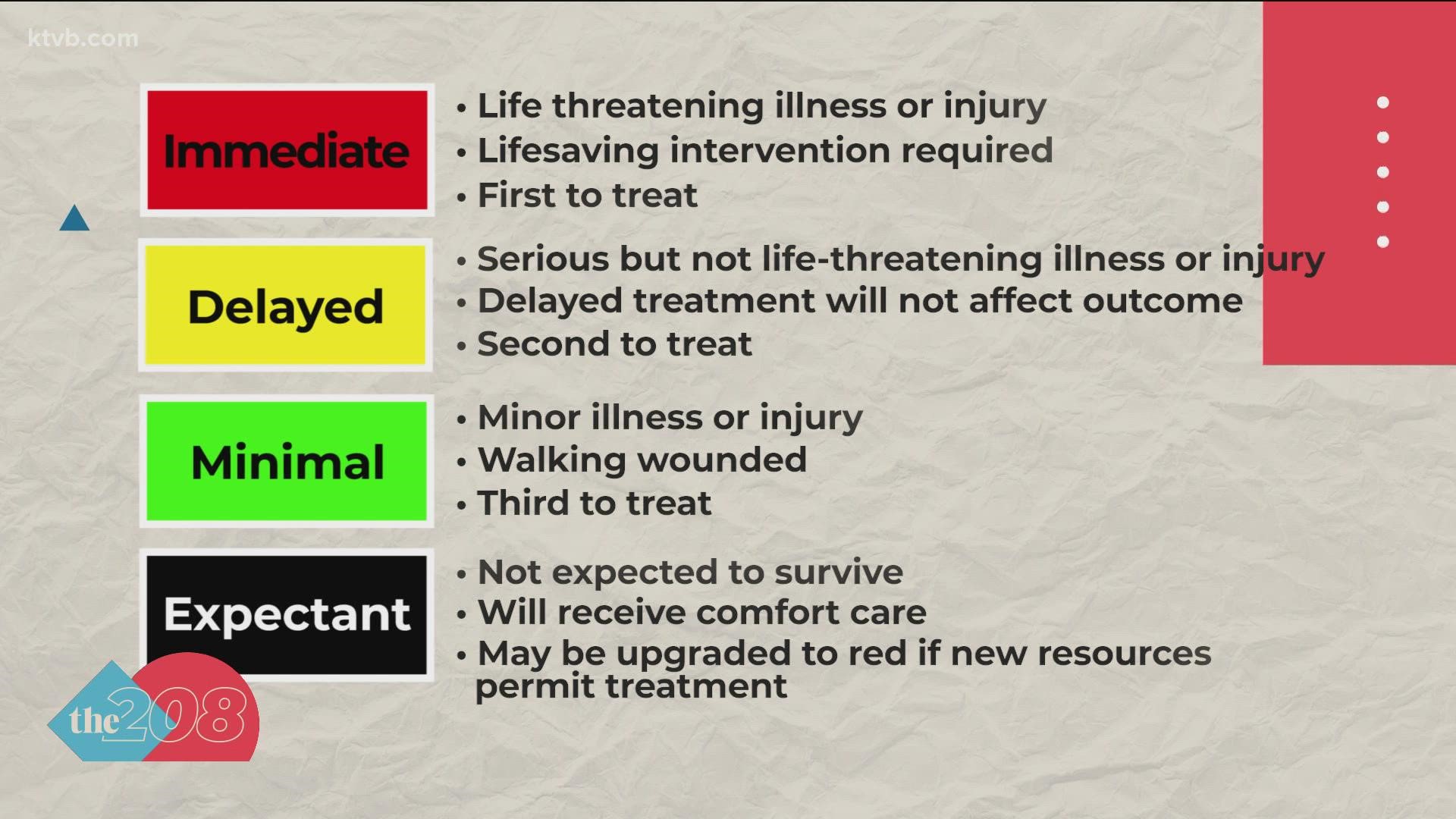
Idaho's health and welfare director has called crisis standards a "last resort." The worst-case scenario would be a situation in which allocation of limited resources would be prioritized based on which patients are deemed more likely to have positive outcomes. More likely, and already happening in some places, is a different level of care.
"That would mean longer wait times to get into a hospital and emergency room, potentially being seen in non-traditional places such as hallways or conference rooms or other spaces at the hospital, or even outside of the hospital," said David Jeppesen, Idaho Health and Welfare director. As he described hospital care scenarios under crisis standards, he also said each nurse would need to see more patients.
Dr. Robert Scoggins, a pulmonary and critical care physician, is the ICU medical director and chief of staff for Kootenai Health in Coeur d'Alene. He joined Idaho Dept. of Health and Welfare officials in a COVID-19 media briefing, which was livestreamed on KTVB.COM and the KTVB YouTube channel.
Scoggins said the number of COVID patients at Kootenai Health has risen from 25 at the beginning of August to 113 on Monday, September 6. Scoggins called Monday's COVID patient population "a significant percentage of our hospital beds."
"We've had a COVID unit since last year, now over year. We've never shut it down. We've never gotten to zero patients. We've always had COVID patients here," Scoggins said. "They're mostly the delta variant, I think, now."
Scoggins said Kootenai Health is seeing significantly more relatively young patients as the delta variant has surged compared to the first couple waves of the COVID pandemic. He said they range from 18 years old to people in their early 80s. Last winter, he said, the majority of Kootenai's COVID patients were over the age of 65. He said about ten percent of the patients are vaccinated, and added that many of them are people who would have difficulty responding to the vaccine because of a suppressed immune system.
"I think the thing that's really changed for us is seeing that younger patients are dying from this, and it's quite disturbing to see these patients declining, and they're what I would consider healthy," Scoggins said. "They're normal, everyday North Idaho people."
While some of those younger patients dying or suffering serious complications from COVID-19 have some comorbidity -- meaning one or more underlying health issues -- Scoggins said Kootenai has seen some with no significant past medical history die or require high amounts of oxygen or ventilation because of the delta variant of COVID.
Of 39 patients in critical care at Kootenai, Scoggins said 19 are on ventilators. The other 20 are on high-flow oxygen, and doctors are concerned that they may also need to go on a ventilator.
"We are converting many wards now into COVID wards for both acute care -- lower level... and then also critical care," Scoggins said. "Normally we have 26 ICU beds in this hospital, and you may be asking how we can handle 39 COVID patients... actually, our total ICU census is right around 50, and that's because we converted about 32 extra beds, usually med-surgical beds, into ICU beds last year in preparation for something like this. It's put an extreme strain on our resources, our nursing -- they're doing team nursing throughout the hospital, where we have one ICU nurse for six patients, and he or she is working with two other nurses to care for those patients to keep the ratios at 1-to-2 (one nurse per two patients)."
Scoggins also said Kootenai recently converted a conference center to house 22 patients.
"It's not obviously an ideal setting. It's a conference room that we've put beds into, it's an open setting with dividers. The staff wears PPE all the time," Scoggins said, adding that the entire third floor of Kootenai Health is housing COVID patients.
Along with Scoggins and Jeppesen, those also speaking and taking questions during the briefing were Elke Shaw-Tulloch, administrator for the Division of Public Health; Dr. Christine Hahn, state epidemiologist; and Dr. Kathryn Turner, deputy state epidemiologist.
Jeppesen said while crisis standards of care are in effect for the state's two northernmost health district, other areas, including the Treasure Valley, have "just a little bit of wiggle room," but not much.
The advisory committee on crisis standards discussed and approved the northern districts' request to activate on Monday evening, and there was "lengthy debate" about whether crisis standards should instead be activated statewide.
"In talking to the rest of the health care entities around the state, they are not quite there," Jeppesen said. "They are really, really close, but they are not quite there."
Shaw-Tulloch said more people getting vaccinated and following protocols such as masking and social distancing can slow the spread of COVID, stem the flow of people going to the hospital, and keep the hospitals from going to crisis standards.
Jeppesen urged all Idahoans to be careful about everything, not just the coronavirus, to help preserve hospital capacity, get North Idaho out of crisis standards, and pull the rest of the state's health care providers back from the brink.
"Wear your seat belt, take medications as prescribed, reconsider high-risk activities that could land you in the hospital, because that's where we are with hospital capacity at this point," Jeppesen said.
As of Monday, Sept. 6, the statewide 14-day moving average of new COVID-19 cases was nearly 933 per day, the highest since Jan. 17.
Idaho's COVID-19 website reports that more than 744,000 people in the state are fully vaccinated, and another 90,000 have received only the first dose of a two-dose Pfizer or Moderna series as of Sept. 7.
Of the more than 834,000 people who've received at least one dose of a COVID-19 vaccine, 3,902 later became infected with the virus. Those "breakthrough cases" amount to less than one-half of one percent of the number of people who've received a vaccine.
More about Idaho COVID-19 case trends, along with an interactive map and timelines, is published each weekday on KTVB.COM.
Facts not fear: More on coronavirus
See our latest updates in our YouTube playlist: